Anja Pastor: Dirk, it is a pleasure to be with you today. Thank you for opening our Expert Series! The first topic will be ‘The relevance of inflammation’.
Firstly, how is inflammation defined?
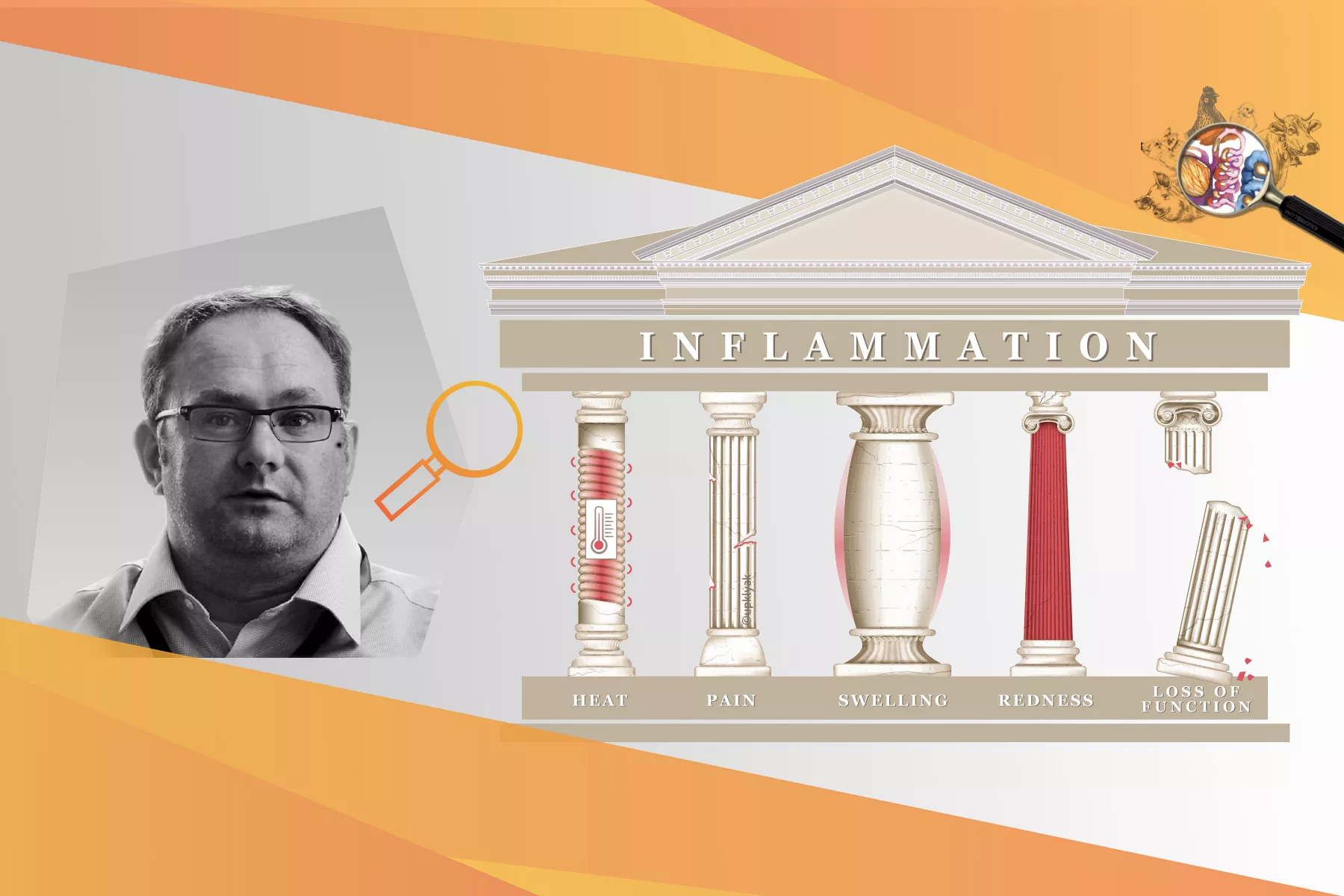
Dirk Werling: Imagine a cut on your skin. You will notice redness, swelling, function loss, heat and pain. These 5 cardinal symptoms are what really defines an acute inflammatory process. This principle is valid for inflammation sites in any part of the body.
AP: Inflammation is part of the innate immune system. If the innate immune system were a human being, what kind of job would it have?
DW: The innate immune system would probably be a standard policeman, always on patrol. In contrast, the adaptive immune system – producing antibodies – is more specialised, some parts very highly specialised – comparable to a firearms unit dealing with terrorists.
AP: Why is inflammation so important that “the policeman” must always be on duty?
DW: We must keep in mind that the immune system is not an ‘On-Off‘-system. The immune system needs to be able to react quickly to any potential threat to protect the body from harm and thereby ensure survival.
Inflammation has 2 major jobs. To alert the immune system that something is happening in a specific organ/tissue that needs to be dealt with and to put the whole body in a pre-warning state. This way, if the damage cannot be contained at that site, we can still protect the remaining organs. This is independent from the site of infection and the transition from a local to a systemic reaction is fluent.
As a result, the whole body participates in making the life of pathogens as uncomfortable as possible. There is for example a change in behaviour: if you are sick, you eat less and energy turnover shifts from sugars to fat. Less oxygen is provided for bacteria and cell survival in general. This principle of inflammation applies to all animals. There are some species-specific factors like different cell receptors, but the general concept is the same.
AP: What can trigger inflammation in livestock?
DW: Inflammation can be triggered by various stressors, especially pathogens and some classical age-dependent events negatively impact the health status of the animal. Weaning stress, for example, is well known to trigger inflammation and to have a negative impact on gut health. Other examples are giving birth or bringing together calves from different farms for fattening. Everything that impacts on the normal function of the tissue can lead to inflammation and this normally goes hand in hand with an infection as the entry of pathogens is facilitated.
AP: Is inflammation also connected to the use of antibiotics?
DW: Definitely. Antimicrobial usage – both given orally or parenterally – leads to a shift in the microbiota on mucosal surfaces like the gut. Especially after the withdrawal of antibiotics the shift in the microbiota can then enable undesired bacteria to manifest and this can cause complications leading to inflammation.
AP: What role does subclinical inflammation play in farm animals?
DW: In subclinical inflammation, the five cardinal signs of inflammation are not seen to the full extent. The affected organ can be slightly painful or uncomfortable, there may be some loss of function, and there is some infiltration with immune cells but not to the extent of an acute inflammation.
Consequences of subclinical inflammation are temporarily impaired growth and feed efficiency in young animals due to ongoing inflammatory processes (e.g., caused by weaning stress).
Mastitis is a good example to show the difference between varying grades of inflammation. With subclinical mastitis, the milk looks normal, but a higher somatic cell count is given. Maybe the udder looks a little bit puffy or is slightly warmer to the touch.
In contrast, if cows face an acute udder infection, the typical milk character is gone and the cow’s udder is very painful and sensitive.
AP: When do we see an overshooting immune response?
DW: In general, immune responses are well orchestrated and finely tuned reactions, neither too weak nor too strong. A good immune response works like an orchestra. Only if all the instruments are in the right place, at the right time, in the right quantity, we get a perfect sound.
One example where this fine-tuned orchestra isn’t working is E. coli mastitis in dairy cows. Here, lipopolysaccharides from the E. coli membrane result in an overreaction of the immune system: The immune cells in the udder are constantly secreting immune modulators, which, rather than preventing more damage, actually increase damage to the tissue.
This can be compared to the conductor forgetting to stop the drums… and they keep on banging! Now, if someone takes away the drumsticks, we can start playing together in harmony again. Or, in the context of the E. coli mastitis, if you can “dampen” the immune response a bit, you give the immune system the chance to work together efficiently and to clear the infection without the negative side effects of an overshooting immune reaction.
AP: So, it makes sense to think about inflammation management.
DW: Definitely, yes. Under practical conditions it is not likely that management, welfare, nutrition, and husbandry can always be spot on. Every tool – a new barn, improved biosecurity, or feed additives – that supports the body to deal with an infection faster or spend less energy and nutrients on a response is very beneficial.
AP: If we contain inflammation, can we be sure that the body is still able to deal with an infection efficiently?
DW: Absolutely yes. Again, the immune system is never switched off. It is just controlled so that it doesn’t overreact but it is able to react as soon as it is needed.
AP: One word that is often mentioned in combination with inflammation is “NF-KB”. Can you explain what it is?
DW: NF-κB stands for “nuclear factor kappa-light chain enhancer of activated B-cells”. It is one of the major transcription factors to switch on the transcription of genes for pro-inflammatory immune modulating cytokines like Interleukin 1 and Tumor Necrosis Factor. NF-κB is expressed in many cells of the body of all animals. Somewhat simplified you can say that if you get poked by someone, the likelihood that the poked cells respond with an NF-κB inflammatory answer is quite high. The same is true for all farm animals.
AP: What is your advice for livestock producers in terms of inflammation?
DW: Where applicable, optimise management, nutrition, and husbandry, and avoid metaphylactic treatment with antibiotics.
AP: Thank you very much for your time and insights, Dirk!
Dirk Werling
Professor of Molecular Immunology, Royal Veterinary College, London, UK
Dirk Werling is a Professor of Molecular Immunology at the Royal Veterinary College, London. Dirk obtained a Dr.med.vet in virology as well as a Ph.D. in immunology. After an Assistant Professorship at the Institute of Virology at the University of Bern, Dirk moved on to the Royal Veterinary College in London where he holds the Chair and Professor in Molecular Immunology. This enables him with the unique opportunity to develop new vaccine-platforms for farm animals by targeting the then (2007) newly discovered class of innate immune receptors, such as the Toll-like receptors.
So far, this work resulted in the submission of 3 different patent-applications, and together with his work group, Dirk has published over 100 peer-reviewed publications, ranging from empirical research topics such as the coevolution between host and pathogens, and the species-specific recognition of patterns to the interaction of the microbiome and the immune system.
Contact our experts or send us a message. We will contact you as soon as possible.